Download the patient handout here
Download the provider’s communication here
We understand the skepticism. But let’s just review the facts.
We were doubtful of the Brain Disease Model of Addiction as it pertains to the opioids. The Brain Disease Model of Addiction as it pertains to the opioids is not based on science. We are only discussing opioids here, not amphetamines, cocaine, nicotine, or any other substance. We are only talking about the opioids.
Our theory is different. You can read more about it here: the
Smith Hypothesis.
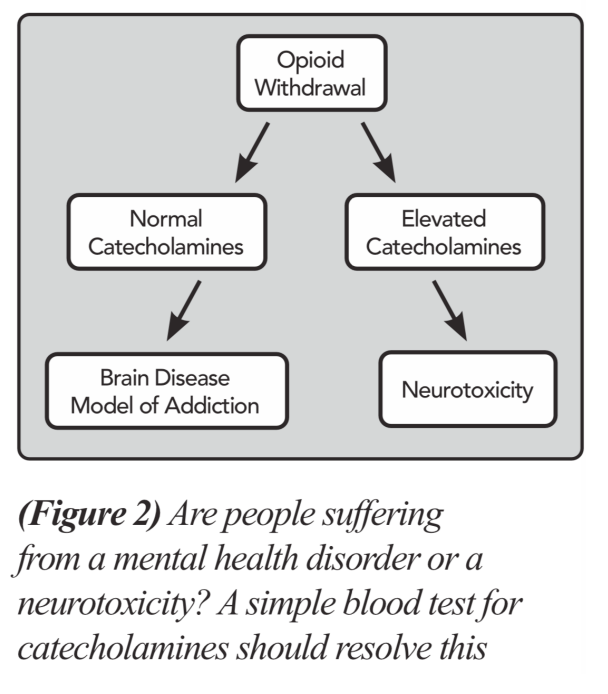
We determined that a simple blood draw from participants in opioid withdrawal would settle the issue. The Brain Disease Model of Addiction did not predict a Catecholamine toxicity to be present during opioid withdrawal.
The Smith Hypothesis did predict a Catecholamine toxicity would be present during opioid withdrawal. This is the first time Catecholamines were measured in humans during an episode of opioid withdrawal due to opioid abstinence.
Here are the results of the first 15 participants in our IRB approved study. These Catecholamine levels were deemed incompatible with life. An emergency halt was imposed and the IRB was notified. Levels elevated are in gray. 13 out of 15 participants had at least one elevated Catecholamine. 6 out of 15 had multiple elevated Catecholamines. 2 participants had a deadly combination of elevated norepinephrine and elevated epinephrine.
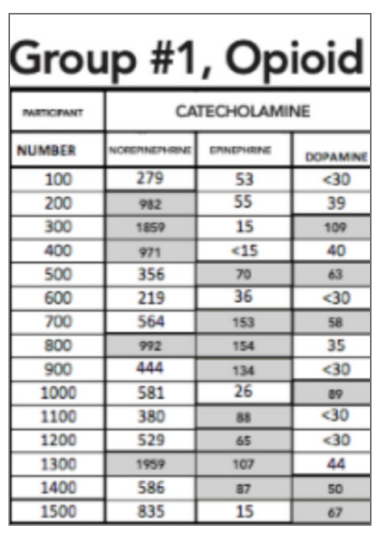
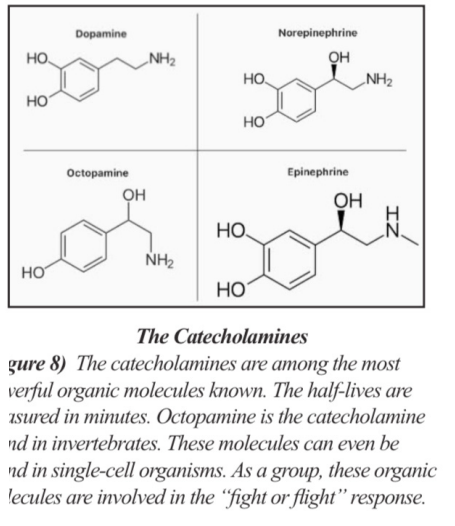
The Catecholamines and the associated “fight or flight” response is interwoven with life itself. But the Catecholamines have a half-life of about two minutes. Our participants had their blood drawn on Day #3 of opioid withdrawal. The horror they had experienced from
days of Catecholamine toxicity and an unrelenting “fight or flight” stimulation simply defied words.
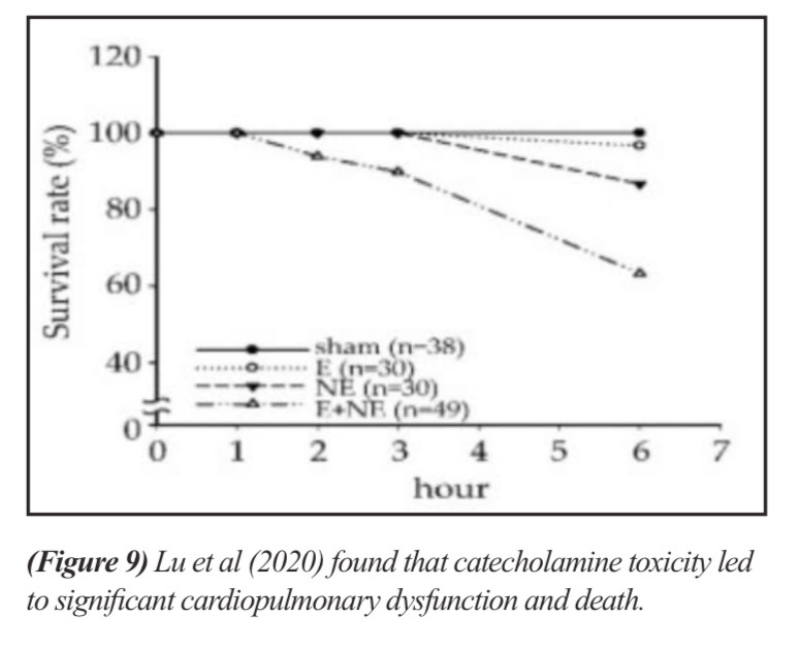
Lu et al (2020), referenced in our article, demonstrated how quickly the Catecholamine Toxicity can kill. Lu did not test dopamine. The combination of norepinephrine and epinephrine toxicity killed the quickest. 2 of our 15 participants had this deadly combination.
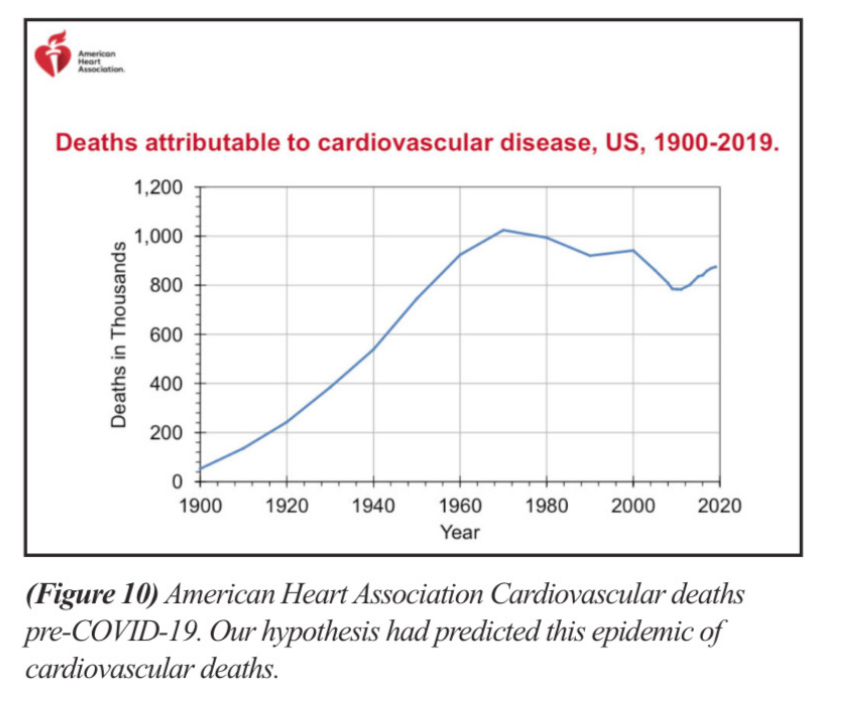
We believe the upward blip in cardiovascular deaths are due to an epidemic of unrecognized and untreated Catecholamine Toxicity.
On autopsy, no opioid would be found. These individuals died during an episode of opioid withdrawal.
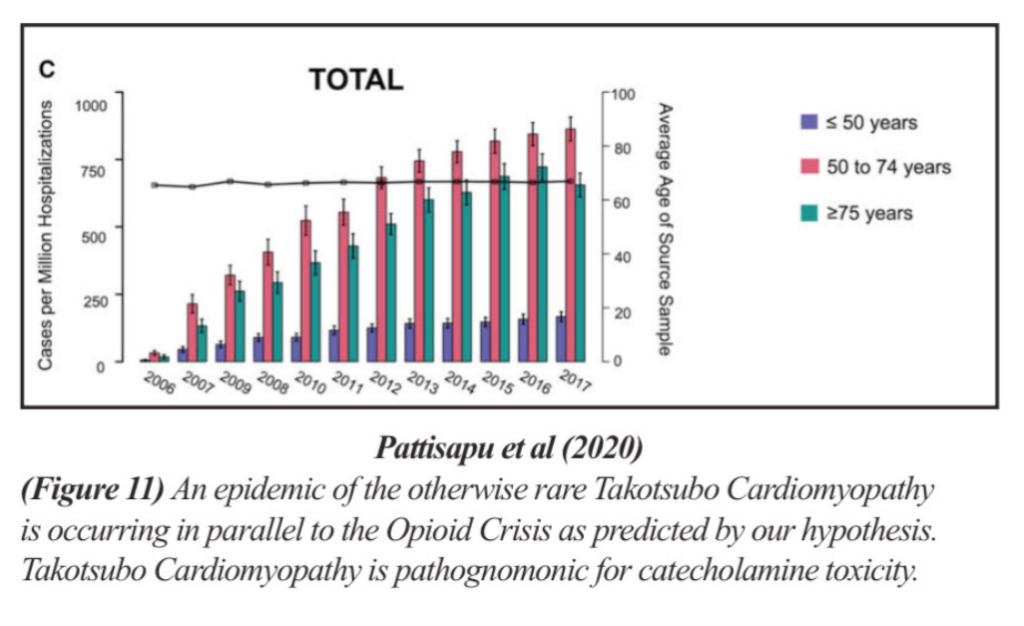
Still skeptical? Then please explain the explosion in the
otherwise rare Takotsubo Cardiomyopathy.
These victims are overwhelmingly older, postmenopausal
women. These are truly tragic events.
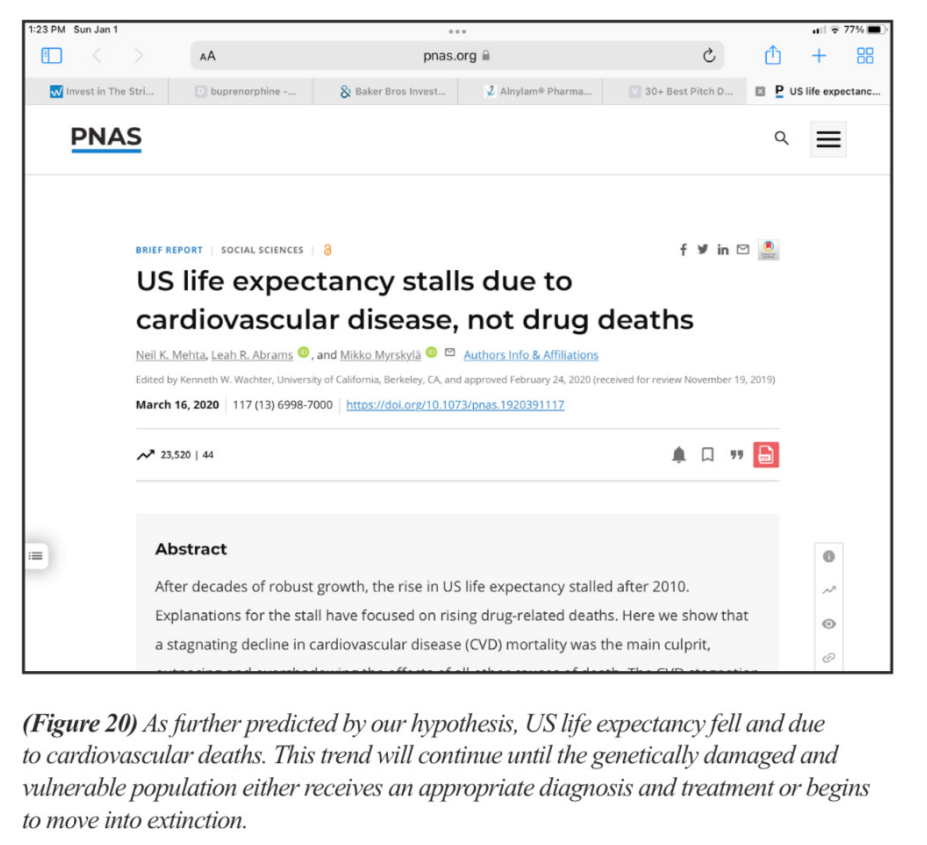
The deaths are of such a magnitude that life expectancy in the United States was impacted.
We anticipate a plethora of wrongful death lawsuits. Many were misdiagnosed. Many had visited a hospital seeking help.
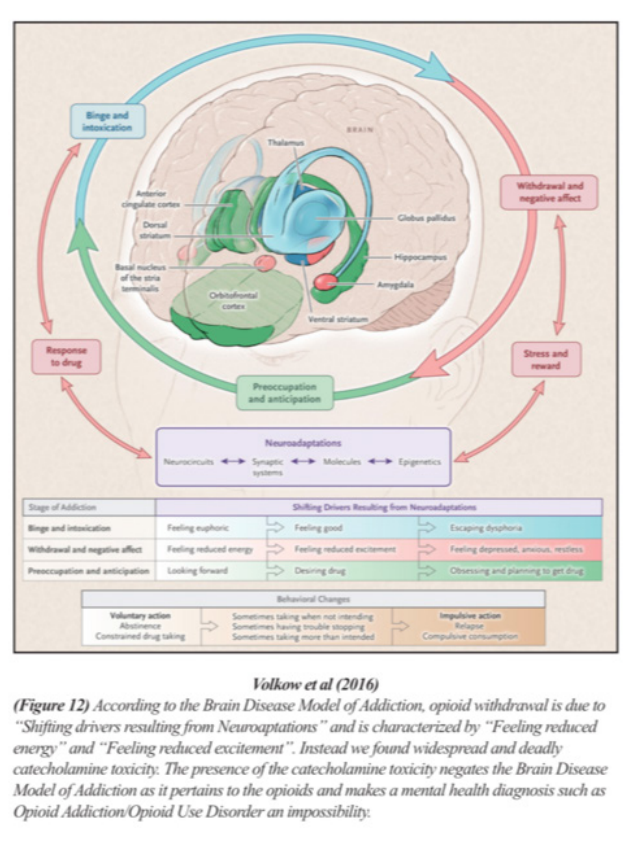
The Brain Disease Model of Addiction describes withdrawal
as a state of “feeling reduced excitement”
This is a representation of the OPRM1 gene. The gene for the mu-opioid receptor. This is results from our DNA analysis of the opioid dependent vs the opioid naive.

Everywhere the red column is bigger than the blue
column is a location of methylation toxicity due to
opioid exposure. Methylation toxicity causes Gene Silencing. What do you think might happen to the mu-opioid receptor that was produced from the OPRM1 gene with this many areas turned off? Do you really believe that this receptor made from this poisoned DNA is going to behave
normally?
We ran our DNA results through Artificial Intelligence.
Artificial intelligence had no problem seeing the two data
groups as completely separate entities.

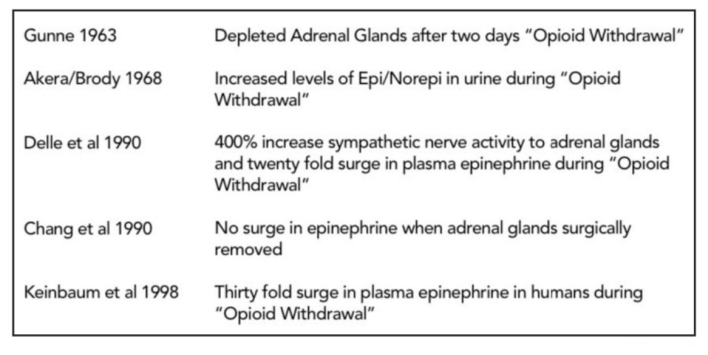
The evidence of a dysfunction involving the adrenal glands is decades old. But when NIDA took over the funding for research beginning in 1992, this field of research simply stopped.
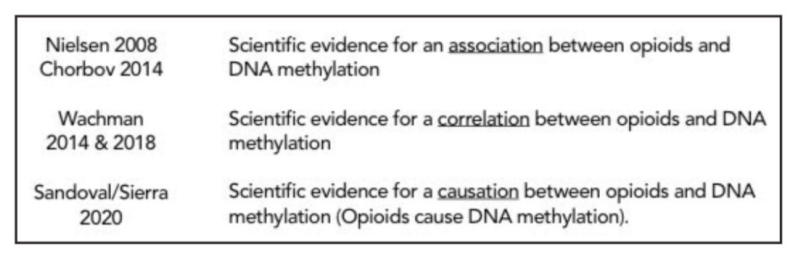
The scientific evidence for a methylation in the DNA associated with the opioids is over 15 years old. A failure to diagnose or delay in diagnosis malpractice case could be
difficult to counter.